By Dr Jorge L. Alió
Over the past 1 O years, an increasing number of studies have been conducted on the topic of keratopigmentation-that is, the induced cosmetic pigmentation change in the cornea.
Keratopigmentation can be done for therapeutic purposes (eg, for cornea! leucomas and blind and disfigured eyes, as well as cases with traumatic aniridia or other problems that affect the eye’s quality of vision).
The topic has been extensively studied and covered in a series of papers that have demonstrated that such techniques are effective, feasible and very useful for patients.
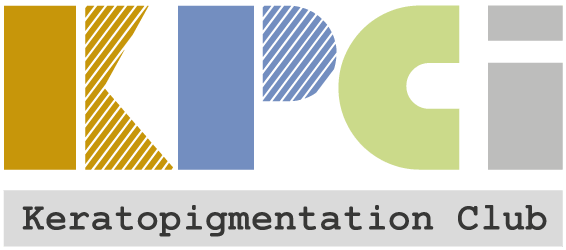
Following this, the purely cosmetic application of this technique has offered the possibility to change the apparent colour of the eye on a voluntary basis. This is purely an aesthetic application that has been obviously disruptive and controversia!. My colleagues and I first described this technique, 7 and it has been practised in Europe by a few surgeons on a continua! but selective basis. The biotolerance and local toxicity of the pigments used in keratopigmentation have been the subject of extensive experimental studies. In Figure 1, we display the instruments used in the modern keratopigmentation surgical technique.
Therapeutic keratopigmentation is indeed a new and relevant type of cornea!
surge1y; however, it is still not in general use, essentially because of the insuffi.cient development of pigments specifically for cornea! use. Patients with disfigured corneas and blind eyes, and patients who prefer not to go through the trauma associated with evisceration and enucleation and their potential complications, find this new type of surge1y to be a very valuable alternative that can successfully restore their appearance in a less invasive manner.
The pigment may be placed inside the cornea! stroma when the superficial cornea is transparent (intrastromal keratopigmentation) (Figure 2). With totally opaque corneas, the technique should be performed by applying the pigment on the cornea! surface (superficial keratopigmentation)
(Figure 3). either manually or using an automatic device (Figure 4). In superficial keratopigmentation, the pigment is injected into the superficial cornea] stroma up to the leve] of 140 µm, after denuding the come! epithelium (Figure 3).
Superficial leucomas are treated with superficial techniques, whereas deep opacities, aniridias and other problems that happen in a patient’s eye are better treated by intralamellar techniques. Surgical instruments and techniques have also been described in detail in other publications.15 (Figures 1 and4).
When the superficial cornea! stroma is transparent, the intrastromal pigmentation technique can be better used. For this purpose, cornea! stromal tunnels are created, assisted by femtosecond laser at the adequate cornea! depth, which also creates a dissection to simulate the pupil at an adequate diameter (Figure 2).
Such cornea! tunnels may also be created manually using adequately designed instruments (Figures 1 and 2).
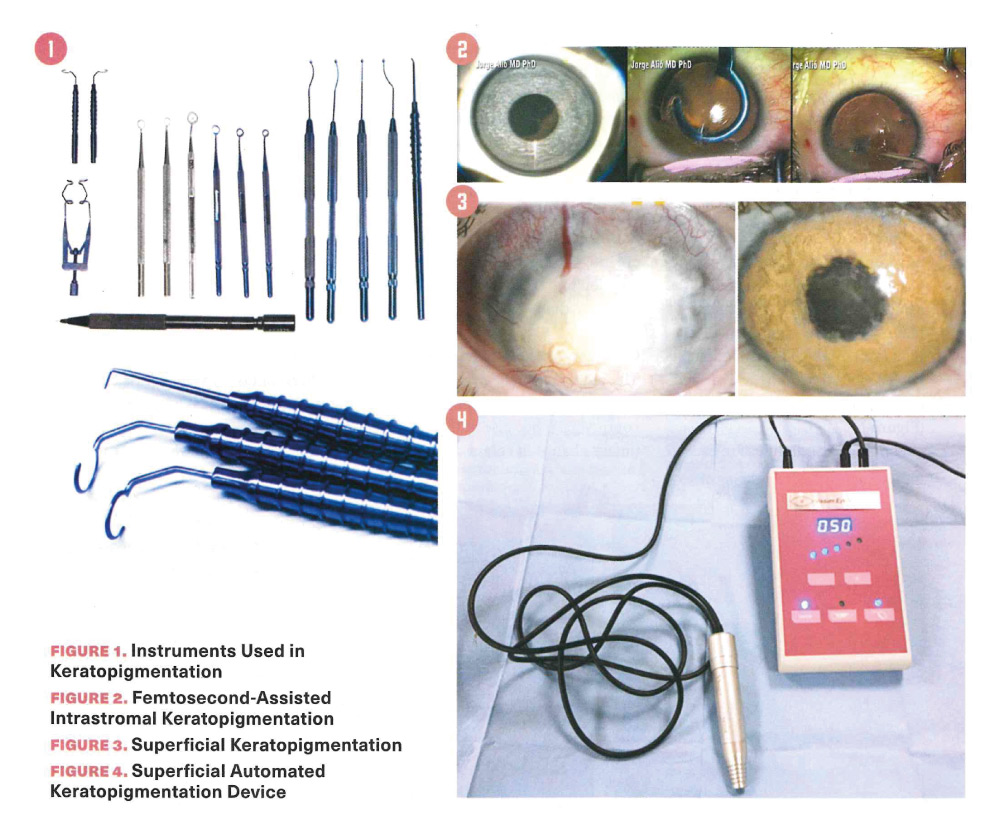
The pigment is matched to the colour of the contralateral normal eye, while the pupil is simulated with black pigment (Figure 5). The main limitation of this technique is the availability of pigments, which are, as of the writing of this article, lirnited to a few colours and labeled for cornea! use with the CE mark. The use of dermatological pigments probably could be acceptable, but the lack of negative effects has not yet been demonstrated on the normal or diseased cornea, as the pigments are made of compounds that are often reactive when in contact with light; thus oxidation may occur. This can lead to a change in the colour over time and might make outcomes of this surgery unpredictable.
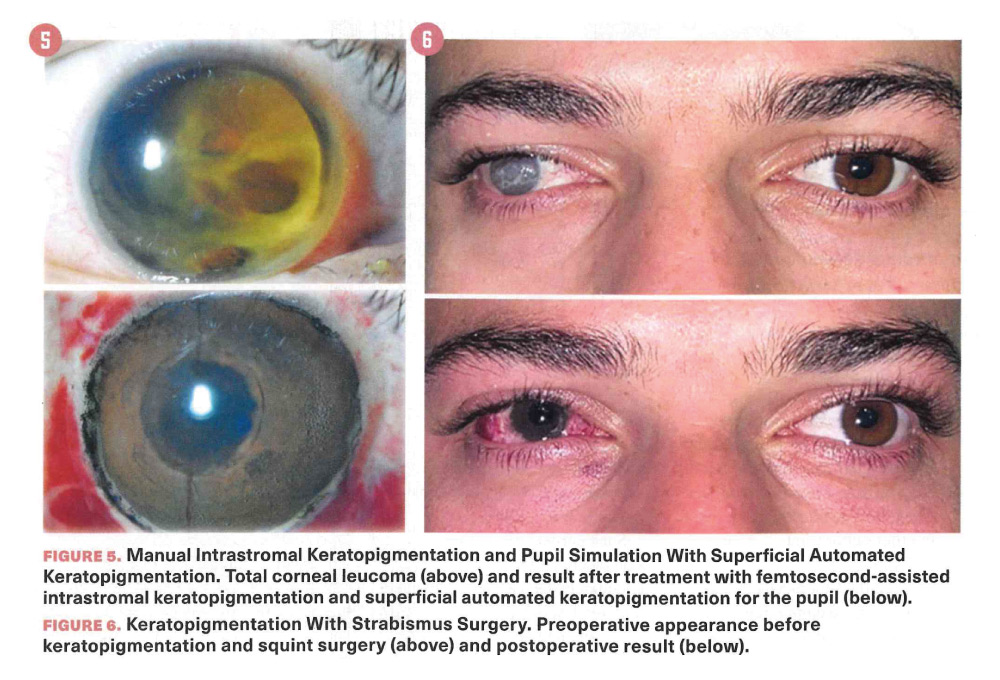
Frequently, severely compromised and blind eyes are associated with other disfiguring features such as squint and ptosis, which can also be successfully corrected at the same time as the keratopigmentation procedure is performed. A high level of patient satisfaction has been reported with the use of such combined surgical techniques (Figure 6).
Functional disabilities are caused by iris problems such as aniridia, iris atrophy and iris colobomas. Sorne oí these cases, which either currently have no solution or require extensive and invasive surgeries, may be approached today with intrastromal keratopigmentation. Even intractable diplopías can be solved with keratopigmentation creating a central scotoma by the creation of a sirnulated pupil oí adequate diameter.
Controversial topic
The purely cosmetic use oí keratopigmentation is disruptive and controversial because oí the voluntary change of colour oí the eye that intrinsically has this problem. The procedure is elective, can be performed inadequately and can lead to complications in normal eyes. With respect to this fact, findings from a recent study demonstrated that keratopigmentation is, undoubtedly, the best option available for those individuals who wish to change the apparent colour oí the eye on a voluntary basis. It demonstrates superior saíety to and better outcomes than the altemative approaches using iris colour prosthesis or laser iris depigmentation procedures, which are affected by myriad severe complications that can lead to severe visual loss and even blindness. In particular, the use oí prosthetic coloured irises should be considered today as a medical malpractice procedure beca use of the proven severe comorbidities that have been demonstrated to be induced by their implantation in the medium and the long term.
Emerging surgical technique
With this in mind, it should be considered that this emerging surgical technique oí keratopigmentation has been refined with the modem development of specific surgical instruments. These include íemtosecond lasers and the modem development oí pigments. However, the comeal pigments used are considered underdeveloped owing to the main limitation oí this technique to be used in general.
Thus, this technique is open to future developments that will be extremely attractive for ophthalmologists, comeal specialists and cosmetic surgeons. It will also be attractive for patients affected by morbidities that affect the cosmetics oí their eyes due to disfiguring comeal leucomas. The procedure will also appeal to patients who desire to change their appearance through the colour oí their eyes, which should be done for good reason and with appropriate selection by their surgeons.
A new comeal surgical perspective is now available with a good level oí published evidence in support. I envision a promising future that will follow this group oí new surgical techniques. This topic will probably progress immensely in the coming years along with the increase in clinician experience and the development oí more appropriate, specific and diverse comeal pigments. l